The mere mention of “spine surgery” can send a shiver down anyone’s spine, pun intended. For many, it conjures images of large incisions, prolonged hospital stays, intense pain, and a long, arduous recovery period. For years, traditional open spine surgery, while effective, did indeed involve significant muscle dissection and tissue disruption, leading to these concerns. But what if I told you that spinal surgery has undergone a remarkable transformation? What if there’s an approach that aims to achieve the same therapeutic goals with significantly less impact on your body? This innovation is known as Minimally Invasive Spine Surgery (MISS), and it has revolutionized how we approach complex spinal conditions.
If you’re grappling with chronic back or neck pain, numbness, weakness, or other debilitating spinal issues, and surgery is being considered, you’re likely asking: what is minimally invasive spine surgery? This approach represents a paradigm shift in spinal care, moving away from extensive incisions towards techniques that prioritize preserving healthy tissue. It’s designed to reduce the trauma to your body, accelerate your recovery, and get you back to your life with less pain and greater mobility. Let’s delve into the world of MISS, understanding its principles, techniques, benefits, and how it’s offering new hope to countless individuals.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult NowDefining the Revolution: What Is Minimally Invasive Spine Surgery?
At its core, what is minimally invasive spine surgery? It’s a collection of advanced surgical techniques and technologies designed to treat spinal conditions through smaller incisions and with less disruption to surrounding muscles and soft tissues compared to traditional open spine surgery. While the ultimate goal of the surgery (e.g., decompressing a nerve, stabilizing the spine) remains the same, the method of accessing the spine is fundamentally different.
The key principle of MISS is to minimize damage to the muscles that support the spine. In traditional open surgery, a long incision is made, and muscles are cut or stripped away from the bone to gain a clear view of the spine. While effective, this muscle damage can lead to more pain, blood loss, longer hospital stays, and a slower recovery. Minimally invasive techniques, on the other hand, utilize specialized instruments and imaging guidance to access the spine by either spreading (rather than cutting) muscle fibers or approaching the spine through natural openings.
Key Differences and Advantages Over Traditional Open Surgery:
Understanding what is minimally invasive spine surgery truly means appreciating its distinct advantages:
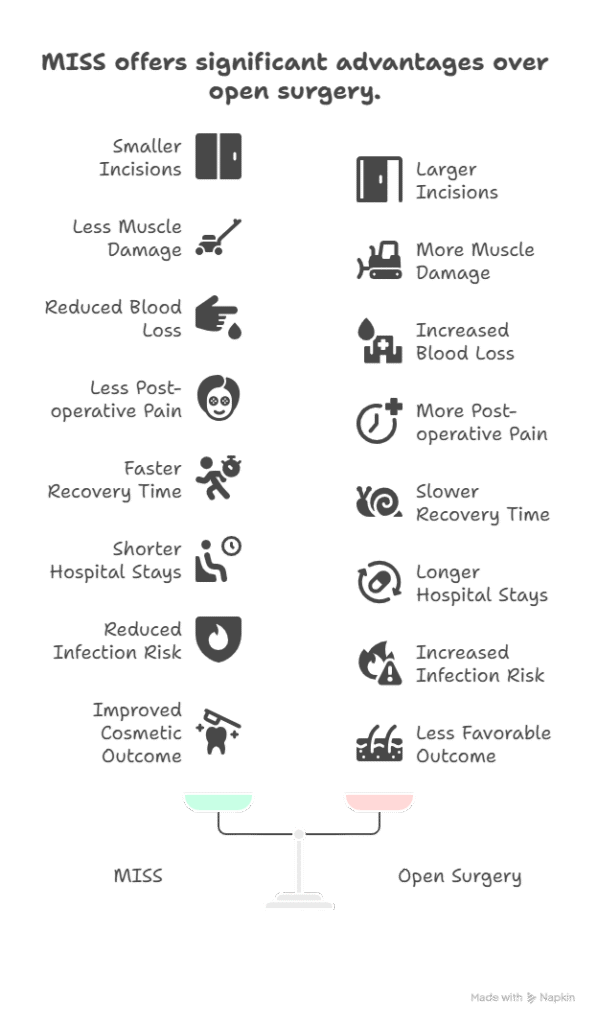
- Smaller Incisions: Instead of a long incision (often 5-6 inches or more), MISS typically involves one or more small incisions, often less than an inch or two in length.
- Less Muscle Damage: This is the most significant advantage. MISS uses dilators and tubular retractors that gently push muscle fibers aside, rather than cutting them. This preserves muscle integrity, reduces post-operative pain, and speeds recovery.
- Reduced Blood Loss: With less tissue trauma and muscle dissection, blood loss during MISS procedures is significantly lower. This often negates the need for blood transfusions.
- Less Post-operative Pain: Because muscles are preserved, patients typically experience less pain after MISS compared to open surgery, requiring less opioid medication.
- Faster Recovery Time: Reduced tissue trauma translates directly into a quicker healing process. Patients often mobilize sooner, return to daily activities faster, and can get back to work or hobbies more rapidly.
- Shorter Hospital Stays: Many MISS procedures can be performed on an outpatient basis or require only a one-night hospital stay, compared to several days for traditional open surgery.
- Reduced Risk of Infection: Smaller incisions mean less exposure to the external environment, significantly lowering the risk of surgical site infections.
- Improved Cosmetic Outcome: The smaller incisions leave smaller, less noticeable scars.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult NowThe Technology and Techniques Behind MISS: Precision and Innovation
The ability to perform what is minimally invasive spine surgery relies heavily on cutting-edge technology and specialized instruments that allow surgeons to work through small openings with enhanced visualization and precision.
- Tubular Retractors: These are perhaps the most defining tools of MISS. After a small incision, a series of progressively wider tubes (dilators) are inserted, gently pushing the muscle tissue aside until a working channel (the tubular retractor) is created. This tube holds the muscles apart, providing the surgeon a direct, narrow view of the spinal structures without cutting the muscle.
- Endoscopes and Microscopes: Once the tubular retractor is in place, an endoscope (a thin, flexible tube with a camera and light source) or a high-powered operating microscope is inserted. These provide magnified, illuminated views of the surgical field, allowing the surgeon to see intricate details through the small opening. Some procedures are entirely endoscopic, meaning the entire surgery is performed through the endoscope.
- Specialized Instruments: Surgeons use long, thin, precisely designed instruments that can fit through the narrow working channel of the tubular retractor. These include dissectors, forceps, drills, and other tools, all meticulously crafted for accuracy in a confined space.
- Intraoperative Imaging: Real-time imaging is crucial for guiding MISS procedures and ensuring precise placement of instruments and implants.
- Fluoroscopy: A real-time X-ray imaging technique that allows the surgeon to see the spine and instruments on a monitor during the procedure.
- O-arm or C-arm: Advanced portable X-ray systems that provide 3D images and allow for navigation, giving surgeons a comprehensive view of the spinal anatomy and instrument trajectories.
- Navigation Systems: Similar to a GPS system, these computer-assisted technologies integrate pre-operative CT or MRI scans with real-time intraoperative imaging. This allows the surgeon to track the exact position of instruments in relation to the patient’s anatomy on a screen, enhancing accuracy and safety, especially when placing screws or performing complex maneuvers.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult NowConditions Treated by Minimally Invasive Spine Surgery:
While not every spinal condition is suitable for a minimally invasive approach, a wide range of common debilitating issues can now be effectively treated with MISS. This means that knowing what is minimally invasive spine surgery could be highly relevant for your potential treatment options.
- Herniated Discs (Microdiscectomy): One of the most common MISS procedures. For a herniated disc that is pressing on a nerve root, a microdiscectomy involves removing the problematic portion of the disc through a small incision, relieving nerve compression.
- Spinal Stenosis (Laminectomy/Decompression): Involves removing bone spurs, thickened ligaments, or parts of the lamina (the back part of the vertebra) to widen the spinal canal and relieve pressure on the spinal cord and nerves. Minimally invasive approaches (e.g., laminotomy, foraminotomy) can achieve this decompression with less disruption.
- Spinal Fusion: This procedure involves permanently joining two or more vertebrae to stabilize the spine and alleviate pain caused by instability or severe degeneration. While traditionally a very invasive procedure, many fusion techniques now have minimally invasive counterparts:
- Transforaminal Lumbar Interbody Fusion (TLIF): Accessed from the back, a tubular retractor is used to remove the disc and insert a bone graft or cage between the vertebrae for fusion.
- Posterior Lumbar Interbody Fusion (PLIF): Similar to TLIF but often involves a slightly different access angle.
- Lateral Lumbar Interbody Fusion (LLIF/XLIF/DLIF): Approaching the spine from the side, through the patient’s flank, to insert the fusion device. This avoids cutting back muscles and can be highly effective for certain levels of the spine.
- Vertebral Compression Fractures (Vertebroplasty/Kyphoplasty): For painful compression fractures, often due to osteoporosis, MISS techniques involve injecting bone cement into the fractured vertebra (vertebroplasty) or first inflating a balloon to restore vertebral height before injecting cement (kyphoplasty). These are very small, needle-based procedures.
- Spinal Deformity Correction (Selected Cases): While extensive spinal deformity correction (like severe scoliosis) often still requires open surgery, minimally invasive techniques are being developed and used for less severe deformities or to stage complex corrections, reducing the overall invasiveness.
- Spinal Tumors or Infections: In selected cases, certain spinal tumors or infections can be managed with minimally invasive approaches to biopsy, remove small lesions, or decompress affected areas.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult NowThe Patient Journey for Minimally Invasive Spine Surgery:
If you’re considering MISS, knowing what is minimally invasive spine surgery is from a patient’s perspective can help prepare you for the journey:
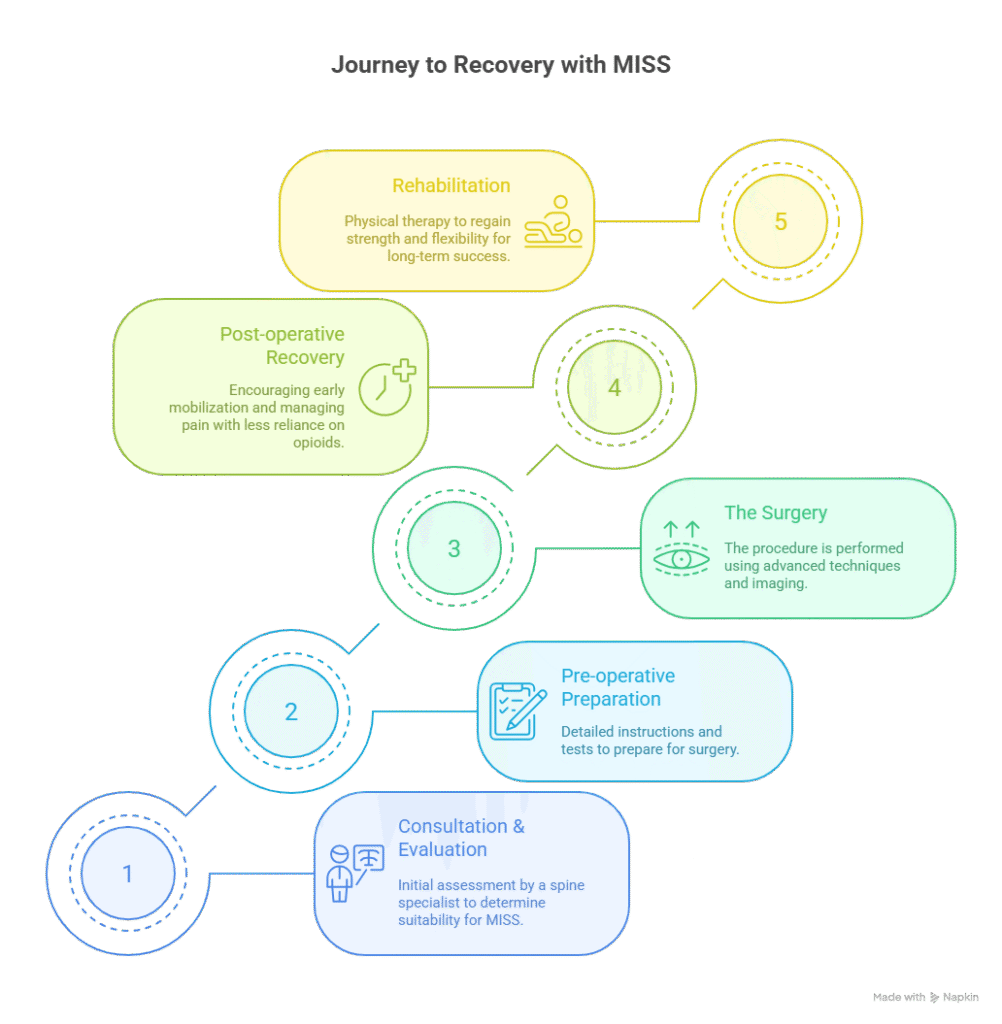
- Consultation and Candidacy Evaluation: Your journey begins with a thorough evaluation by a spine specialist, often a neurosurgeon or orthopedic spine surgeon. They will review your medical history, perform a physical examination, and meticulously analyze your imaging scans (MRI, CT, X-rays). It’s crucial to determine if your specific condition is suitable for MISS, as not all cases are.
- Pre-operative Preparation: Once deemed a candidate, you’ll receive detailed instructions regarding medications to stop, pre-operative tests, and preparations for surgery.
- The Surgery: The procedure is performed under general anesthesia. The surgeon makes small incisions, uses dilators and tubular retractors to create the working channel, and then performs the necessary procedure using specialized instruments and advanced imaging guidance.
- Post-operative Recovery: Due to the reduced tissue trauma, recovery is often faster. You’ll typically be encouraged to mobilize (walk) soon after surgery. Pain management will be provided, often with less reliance on opioids.
- Rehabilitation: Physical therapy usually plays a vital role in recovery, helping you regain strength, flexibility, and proper body mechanics to ensure a successful long-term outcome.
Who Is a Candidate for Minimally Invasive Spine Surgery?
While the benefits of MISS are appealing, it’s essential to understand that not everyone is a candidate. The suitability for what is minimally invasive spine surgery depends on several factors:
- Diagnosis: The specific spinal condition (e.g., herniated disc, stenosis, instability) and its severity.
- Anatomy: The location and characteristics of the spinal problem.
- Overall Health: Patient’s general health, presence of other medical conditions.
- Surgeon’s Expertise: The individual surgeon’s experience and proficiency with MISS techniques.
Complex cases, extensive fusions, severe deformities, or revision surgeries might still require a traditional open approach. Your surgeon will discuss the best option for your specific situation.
Potential Risks and Limitations:
While MISS offers many advantages, it’s still surgery, and all surgeries carry inherent risks. These can include:
- Infection: Though lower than open surgery, still a possibility.
- Bleeding: Though reduced, still can occur.
- Nerve Damage: Potential for injury to spinal nerves or spinal cord.
- Anesthesia Risks: Reactions to anesthesia.
- Persistent Pain: Surgery doesn’t guarantee complete pain relief.
- Recurrence: The original problem (e.g., disc herniation) can sometimes recur.
- Conversion to Open Surgery: In rare cases, if unexpected complications arise or the minimally invasive approach proves insufficient, the surgeon may need to convert to a traditional open procedure during surgery.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult NowFrequently Asked Questions (FAQs)
Is Minimally Invasive Spine Surgery less effective than traditional open surgery?
No, in appropriate cases, Minimally Invasive Spine Surgery is often as effective as traditional open surgery in achieving the surgical goals, but with the added benefits of reduced pain, less blood loss, and a faster recovery due to less tissue disruption.
Does Minimally Invasive Spine Surgery always mean I’ll go home the same day?
While many Minimally Invasive Spine Surgery procedures, especially discectomies or decompressions, can be performed on an outpatient basis, some may still require an overnight stay or longer, depending on the complexity of the surgery and your recovery.
Are all spine surgeons trained to perform Minimally Invasive Spine Surgery?
Yes, physical therapy is almost always a crucial part of recovery after Minimally Invasive Spine Surgery. It helps you regain strength, flexibility, and proper movement patterns, ensuring you achieve the best possible long-term outcome and prevent future issues.
What is the biggest advantage of choosing Minimally Invasive Spine Surgery?
The biggest advantage of choosing Minimally Invasive Spine Surgery is significantly reduced muscle and soft tissue damage compared to traditional open surgery. This leads to less post-operative pain, faster recovery times, and a quicker return to normal activities for suitable candidates.
Can minimally invasive techniques be used for complex spinal problems like severe scoliosis?
While Minimally Invasive Spine Surgery has expanded to treat a wide range of conditions, very complex spinal problems, such as severe scoliosis or extensive multi-level instability, may still require traditional open surgery or a hybrid approach, as MISS might not provide sufficient access or visualization for these extensive corrections.
Embracing the Future of Spinal Care
The advancements in minimally invasive spine surgery have truly transformed the landscape of spinal treatment, offering a less daunting and often more efficient path to recovery for countless individuals suffering from debilitating back and neck conditions. It represents a significant step forward, allowing patients to benefit from surgical intervention with reduced apprehension and improved outcomes.
If you are struggling with chronic spinal pain and considering surgical options, understanding what is minimally invasive spine surgery and whether it’s suitable for your condition is a vital discussion to have with your healthcare provider. For expert evaluation and treatment in advanced neurosurgical and spinal procedures, including complex minimally invasive techniques, consulting with a highly experienced specialist is paramount. Dr. Arun Saroha, a distinguished neurosurgeon, is renowned for his extensive expertise in complex brain and spine disorders, including a profound specialization in state-of-the-art minimally invasive spine surgery. His commitment to precision, patient safety, and personalized care ensures that you receive the most advanced and appropriate treatment tailored to your specific needs, guiding you towards a life with greater comfort and mobility.
Struggling with Back or Spine Pain?
Minimally Invasive Spine Surgery can relieve pain, ensure faster recovery, and help you return to normal life quickly.
Consult Now