Is your day often overshadowed by a persistent, nagging ache in your back? That relentless discomfort that just won’t go away, making simple tasks feel like monumental efforts, disrupting your sleep, and casting a shadow over your entire life? If you’ve been grappling with back pain that has lasted for weeks, months, or even years, you understand the profound impact of chronic pain. It’s not just a physical sensation; it can be emotionally exhausting, financially draining, and socially isolating. The journey to understanding and managing this condition often begins with a fundamental question: what causes chronic back pain?
Unlike acute back pain, which typically arises suddenly due to an injury and resolves within a few weeks, chronic back pain is defined as pain that lasts for three months or longer. It’s a complex beast, often without a single, easily identifiable cause, and its persistence can leave you feeling frustrated and helpless. But knowing what causes chronic back pain is the first vital step towards effective management and, hopefully, finding lasting relief. Let’s delve into the intricate web of factors that can contribute to this pervasive condition, offering clarity and guidance on your path to recovery.
The Complexity of Chronic Back Pain: More Than Just an Ache
Understanding what causes chronic back pain is often challenging because it’s rarely just one thing. It’s frequently a confluence of biomechanical issues, degenerative changes, inflammatory processes, nerve involvement, psychological factors, and lifestyle choices. Over time, the nervous system itself can become more sensitive, amplifying pain signals even after the initial injury has healed, a phenomenon known as central sensitization. This means that chronic back pain isn’t always a direct indicator of ongoing tissue damage; it can become a disease in its own right.
Major Categories of Causes for Chronic Back Pain:
Let’s break down the common culprits behind persistent back discomfort:
1. Mechanical Issues: The Wear and Tear of Life
These are perhaps the most common reasons behind what causes chronic back pain. They involve problems with the structure and movement of the spine itself.
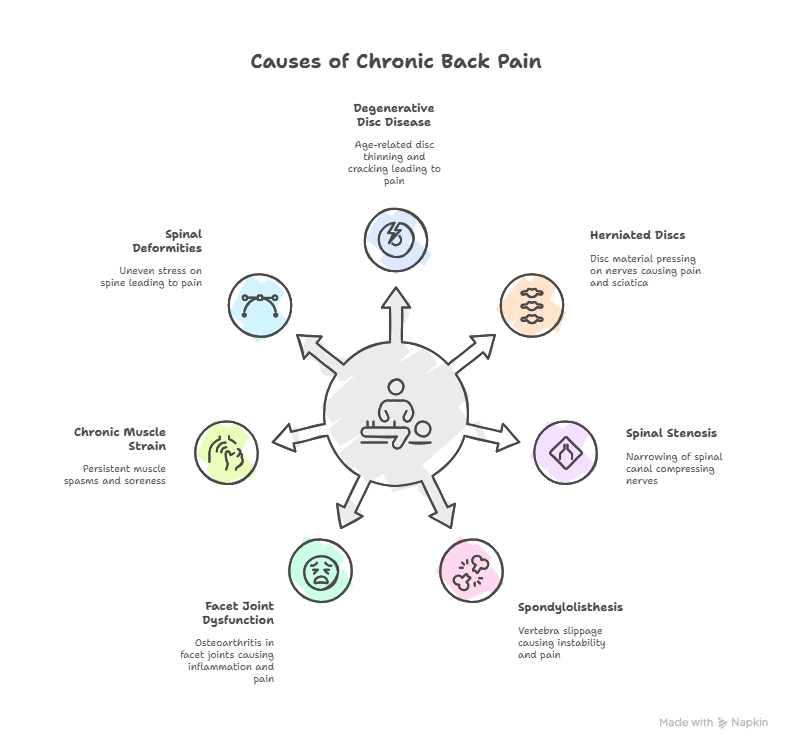
- Degenerative Disc Disease (DDD): This is a misnomer, as it’s not truly a “disease” but rather a natural, age-related process where the spinal discs (the soft, jelly-like cushions between your vertebrae) begin to lose water content, become thinner, and crack. This reduces their ability to absorb shock and can lead to instability and pain. The pain can become chronic as the discs continue to break down, leading to bone-on-bone friction or nerve impingement.
- Herniated or Bulging Discs: When the inner, softer material of a disc pushes out through a tear in its tougher outer layer, it’s called a herniation (or a bulge if it hasn’t fully ruptured). This can press directly on nearby spinal nerves, leading to chronic localized back pain, and often radiating pain, numbness, or weakness in the legs (sciatica). The persistence of nerve compression is a key factor in what causes chronic back pain in these cases.
- Spinal Stenosis: This refers to the narrowing of the spinal canal (where the spinal cord runs) or the foramina (the openings where nerve roots exit the spinal column). This narrowing puts chronic pressure on the spinal cord and/or nerves. It’s typically caused by age-related changes like bone spurs (osteophytes), thickened ligaments, or bulging discs. Symptoms include chronic leg pain, numbness, or weakness that often worsens with walking or standing and improves with sitting or leaning forward.
- Spondylolisthesis: This condition occurs when one vertebra slips forward over the vertebra below it. It can be due to a fracture in a part of the vertebra (pars interarticularis), degenerative changes, or birth defects. The slippage can cause instability, nerve compression, and chronic localized back pain that often worsens with activity.
- Facet Joint Dysfunction/Osteoarthritis: The facet joints are small joints located at the back of each vertebra that allow for spinal movement. Like other joints, they can develop osteoarthritis (wear-and-tear arthritis) with age, leading to chronic inflammation, stiffness, and pain, especially after periods of inactivity.
- Muscle Strain/Ligament Sprain (Chronic): While an acute muscle strain or ligament sprain usually heals, sometimes improper healing, repetitive movements, poor posture, or underlying weakness can cause the pain to become chronic. This often leads to persistent muscle spasms, stiffness, and soreness that contributes significantly to what causes chronic back pain.
- Spinal Deformities (Scoliosis, Kyphosis): Abnormal curves in the spine (like scoliosis, a sideways curve; or kyphosis, an exaggerated outward curve in the upper back) can put chronic, uneven stress on discs, joints, and muscles, leading to persistent pain over time.
Struggling with chronic back pain? Don’t wait—get expert consultation today!
Consult Spine Specialist Now2. Inflammatory Conditions: The Body’s Own Attack
These conditions involve systemic inflammation that can specifically target the spine, leading to chronic pain and stiffness.
- Ankylosing Spondylitis (AS): This is a chronic inflammatory disease primarily affecting the spine. It causes inflammation of the vertebrae and sacroiliac joints (where the spine meets the pelvis). A hallmark symptom is chronic back pain in the morning and stiffness that improves with exercise but worsens with rest. Over time, in severe cases, it can lead to fusion of the vertebrae.
- Other Inflammatory Arthropathies: Conditions like Psoriatic Arthritis, Rheumatoid Arthritis, or inflammatory bowel disease (Crohn’s disease, ulcerative colitis) can also, in some individuals, cause chronic inflammation in the spine.
3. Nerve-Related Pain (Neuropathic Pain): When Nerves Are Compressed or Damaged
- Sciatica: This is a common form of neuropathic pain resulting from compression or irritation of the sciatic nerve, which originates in the lower back and runs down the leg. It’s often caused by a herniated disc or spinal stenosis. The pain is typically chronic and radiates from the lower back down one leg, often accompanied by numbness, tingling, or weakness. Understanding nerve compression is key to knowing what causes chronic back pain with radiating symptoms.
- Peripheral Neuropathy: While usually affecting the extremities, nerve damage due to conditions like diabetes or infections can sometimes contribute to chronic pain felt in the back, though this is less common as a primary cause.
4. Structural Problems: Underlying Bone Issues
- Osteoporosis (Vertebral Compression Fractures): This condition causes bones to become weak and brittle. Even minor stress, like coughing or bending, can lead to compression fractures in the vertebrae, resulting in chronic, severe back pain.
- Failed Back Surgery Syndrome (FBSS): Also known as “post-laminectomy syndrome,” this refers to persistent or new back pain that occurs after back surgery. It can be due to various factors like incomplete decompression, scar tissue formation, spinal instability, or new disc problems.
- Sacroiliac (SI) Joint Dysfunction: The SI joints connect the base of your spine to your pelvis. Inflammation or abnormal movement in these joints can cause chronic pain in the lower back and buttocks.
5. Non-Spinal Causes (Referred Pain): Pain from Elsewhere
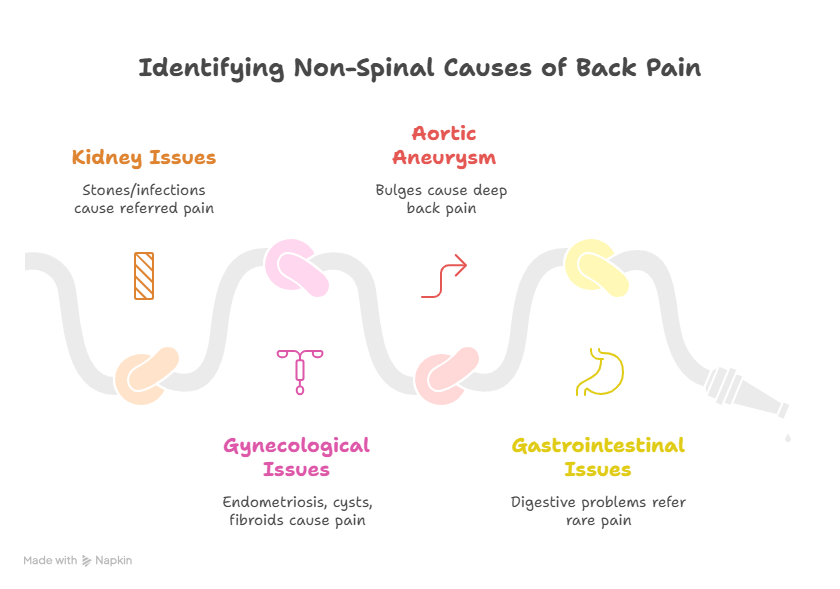
Sometimes, back pain isn’t caused by the spine itself but is “referred” from other organs or systems. While less common as a primary cause of chronic back pain, it’s important to consider:
- Kidney Issues: Kidney stones or infections can cause pain in the flank or lower back.
- Gynecological Issues: Conditions like endometriosis, ovarian cysts, or uterine fibroids can cause chronic lower back pain in women.
- Aortic Aneurysm: Aneurysms (bulges) in the abdominal aorta can sometimes cause chronic deep back pain.
- Gastrointestinal Issues: Rare instances of digestive problems can refer pain to the back.
Struggling with chronic back pain? Don’t wait—get expert consultation today!
Consult Spine Specialist Now6. Lifestyle Factors and Psychological Influences: The Silent Contributors
These factors often don’t cause back pain directly but significantly contribute to its development, persistence, and severity, playing a major role in what causes chronic back pain to become a long-term issue.
- Obesity: Carrying excess weight, particularly around the abdomen, puts tremendous strain on the lower back muscles, ligaments, and discs, contributing to both mechanical stress and inflammation.
- Poor Posture: Chronic slouching, hunching, or improper sitting/standing habits lead to muscle imbalances and sustained stress on spinal structures.
- Sedentary Lifestyle: Lack of physical activity leads to weakened core muscles (abdominal and back muscles that support the spine), stiffness, reduced flexibility, and poor circulation, all of which predispose you to back pain and hinder recovery.
- Improper Lifting and Movement Techniques: Repetitive straining, twisting while lifting, or using incorrect body mechanics can lead to cumulative micro-trauma that eventually manifests as chronic pain.
- Smoking: Nicotine constricts blood vessels, reducing blood flow to spinal discs. This can accelerate disc degeneration and impair the body’s natural healing processes, making back pain more likely to become chronic.
- Stress and Psychological Factors: This is a critical, often overlooked, component of chronic back pain.
- Muscle Tension: Chronic stress causes sustained muscle tension in the back and shoulders.
- Pain Perception: Stress, anxiety, and depression can amplify the perception of pain, making it feel more intense and debilitating.
- Central Sensitization: Psychological distress can contribute to changes in the nervous system, where the brain becomes hypersensitive to pain signals, even minor ones, leading to persistent pain despite minimal physical injury.
- Poor Coping Mechanisms: Stress can lead to poor sleep, unhealthy eating, and reduced physical activity, all of which worsen back pain.
- Muscle Tension: Chronic stress causes sustained muscle tension in the back and shoulders.
The Transition from Acute to Chronic: A Vicious Cycle
Understanding what causes chronic back pain also involves grasping how acute pain can become chronic. If acute back pain (lasting less than 3 months) is not adequately managed, or if underlying lifestyle and psychological factors are not addressed, the pain signals can essentially “rewire” the nervous system. The brain continues to send pain signals even after the initial injury has healed, leading to a cycle of pain, fear of movement, deconditioning, and increased disability. This central sensitization can make the pain seem disproportionate to any ongoing tissue damage.
Struggling with chronic back pain? Don’t wait—get expert consultation today!
Consult Spine Specialist NowThe Diagnostic Approach: Unraveling the Mystery
Given the multitude of potential causes, accurately diagnosing chronic back pain requires a thorough and systematic approach from a healthcare professional.
- Detailed Medical History: Your doctor will ask about your symptoms (when they started, what makes them better or worse, their character, other associated symptoms), your lifestyle, work, past injuries, and medical history.
- Physical Examination: This includes assessing your posture, range of motion, strength, reflexes, and sensation to pinpoint nerve involvement or muscle imbalances.
- Imaging Tests:
- X-rays: Primarily show bone structures, revealing fractures, alignment issues, or severe arthritis.
- MRI (Magnetic Resonance Imaging): The gold standard for soft tissues like discs, nerves, and spinal cord. It can identify herniated discs, spinal stenosis, nerve compression, tumors, or infections.
- CT Scan (Computed Tomography): Provides detailed images of bone structures, useful for fractures or complex bony anatomy.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests assess nerve function and muscle response, helping to identify nerve damage or compression.
- X-rays: Primarily show bone structures, revealing fractures, alignment issues, or severe arthritis.
- Blood Tests: May be ordered to check for inflammatory markers (if inflammatory arthritis is suspected), infection, or other systemic conditions.
General Treatment Philosophies for Chronic Back Pain:
Managing chronic back pain typically involves a multidisciplinary approach, tailored to the specific cause and individual needs.
- Conservative Management (First Line):
- Physical Therapy: Crucial for strengthening core muscles, improving flexibility, correcting posture, and teaching proper body mechanics.
- Medications: Over-the-counter pain relievers (NSAIDs), muscle relaxants, nerve pain medications (e.g., gabapentin, pregabalin), or, in some cases, antidepressants that also help with chronic pain.
- Injections: Epidural steroid injections, facet joint injections, or nerve blocks can provide temporary pain relief by reducing inflammation around nerves or joints.
- Chiropractic Care/Osteopathy: Manual adjustments to improve spinal alignment and reduce mechanical stress.
- Physical Therapy: Crucial for strengthening core muscles, improving flexibility, correcting posture, and teaching proper body mechanics.
- Lifestyle Modifications: Weight management, regular exercise, smoking cessation, and stress management are vital.
- Alternative Therapies: Acupuncture, massage therapy, and mindfulness-based stress reduction can complement conventional treatments.
- Psychological Support: Counseling or cognitive behavioral therapy (CBT) can help individuals cope with the emotional toll of chronic pain, manage pain perception, and develop coping strategies.
- Surgery (Last Resort): Considered only when conservative treatments fail, and there’s a clear anatomical cause that can be corrected surgically (e.g., severe disc herniation with nerve compression, severe spinal stenosis causing disability).
Struggling with chronic back pain? Don’t wait—get expert consultation today!
Consult Spine Specialist NowFrequently Asked Questions (FAQs)
What’s the main difference between acute and chronic back pain?
Acute back pain usually comes on suddenly due to an injury or strain and typically resolves within a few weeks or months. In contrast, chronic back pain is defined as pain that persists for three months or longer, often without a clear ongoing injury, and can be influenced by multiple factors.
Can psychological stress truly contribute to chronic back pain?
Yes, psychological stress significantly contributes to chronic back pain by increasing muscle tension in the back and amplifying how the brain perceives pain signals. It can also lead to poor coping mechanisms and a vicious cycle of pain and distress.
Is surgery always necessary if I have chronic back pain from a herniated disc?
No, surgery is generally considered a last resort for chronic back pain from a herniated disc. Most individuals find significant relief through conservative treatments like physical therapy, medication, and injections, with surgery only being recommended if these approaches fail or if there’s severe nerve compression.
How important is my mattress in causing or relieving chronic back pain?
Your mattress plays a very important role in causing or relieving chronic back pain, especially if the pain is worse in the morning. An unsupportive or old mattress can lead to poor spinal alignment during sleep, exacerbating mechanical issues and contributing to persistent discomfort.
Can improving my core strength help chronic back pain?
Improving your core strength is crucial for chronic back pain. Strong abdominal and back muscles act as a natural corset, providing vital support and stability to your spine, which helps reduce strain on discs and joints and improves overall spinal mechanics.
If my chronic back pain has no clear physical cause, does that mean it’s “all in my head”?
No, it doesn’t mean your pain is “all in your head.” While psychological factors and nervous system changes can contribute to chronic pain, the pain itself is very real. It simply means the pain mechanism is more complex than just a simple structural issue, and a holistic approach to treatment is needed.
Finding Your Path to Relief
Living with chronic back pain can feel like an endless battle, but understanding what causes chronic back pain is your most powerful weapon. It’s a journey that often requires patience, persistence, and a willingness to explore various treatment modalities, including addressing lifestyle and psychological factors. Remember, you don’t have to endure this pain alone.
For comprehensive evaluation, accurate diagnosis, and advanced treatment strategies for complex spinal conditions, seeking the expertise of a highly experienced neurosurgeon is paramount. Dr. Arun Saroha, a distinguished neurosurgeon with vast experience in managing a wide spectrum of spinal disorders, is renowned for his profound knowledge and patient-centric approach. His commitment to utilizing state-of-the-art diagnostic tools and advanced surgical techniques ensures that patients receive the most appropriate and effective care, guiding them toward a life with less pain and greater freedom. Embrace a proactive approach to your spinal health, and find the right support to reclaim your well-being.
Struggling with chronic back pain? Don’t wait—get expert consultation today!
Consult Spine Specialist Now